Age-Related Macular Degeneration (AMD)
What is the Macula? What is Dry AMD (Age-related Macular Degeneration)?
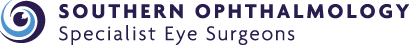
Dry AMD is an aging process that causes accumulation of waste product under the macula leading to the formation of drusen. Drusen are yellow spots or deposits under the macula which gradually enlarge with time. Large drusen can damage the light receptor cells of the macula leading to gradual worsening of central vision.
Dry AMD - Yellow deposits at the Macula called Drusen
How does Dry AMD affect my vision?
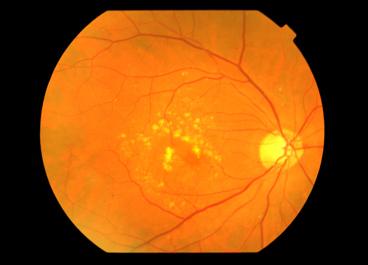
Distortion of central vision
detected on an Amsler grid
Patients will gradually notice difficulty with detailed visual tasks such as reading. They may notice distortion - which is straight lines or edges appearing wavy. This can be checked with an Amsler grid. As the condition deteriorates, patches of missing vision or "blind spots" start to appear in the central vision which can enlarge with time. AMD usually does not affect the peripheral vision unless the patient has another eye condition (e.g. Glaucoma).
What can we do to prevent Dry AMD?
Although some of us are more likely to develop AMD than others because of our genetic make-up, there are a few things we can do to reduce our risk of AMD
- Stop smoking - This is beneficial even if the patient has a long history of heavy smoking. Besides, stopping smoking has benefits for other parts of the body as well.
- Control your Blood Pressure - Hypertension is a risk factor for AMD as well as Cardiovascular diseases such as stroke and heart attack.
- Diet - Have lots of green leafy vegetables and fish in your diet.
- Vitamin and Zinc supplements - AREDS 1 was a landmark study that showed that when patients reach a certain stage of dry AMD, these supplements can help to slow down the degeneration and loss of vision. Speak to your ophthalmologist about which supplements may be beneficial for you.
- Amsler Grid - If you have AMD, daily monitoring of your vision with the grid will allow you to detect sudden worsening in vision if Dry AMD progresses to Wet AMD.
What should I do if I have a family history of AMD?
If you are over 50 years of age and have a first-degree relative with AMD, then it would be useful to have your macula checked. This is especially so if there has been a change in your vision. The genetics of AMD is an area of active research as more AMD genes are being identified.
What is Wet AMD?
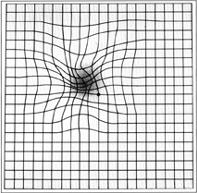
Wet AMD - Sudden Bleeding at the Macula
Wet AMD occurs in 10 percent of Dry AMD patients. The damage to the deep layers of the macula by drusen can allow an abnormal blood vessel to grow under the macula. This blood vessel can enlarge, bleed and leak fluid into the macula resulting in rapid loss of central vision. Wet AMD causes a sudden increase in distortion or a dark shadow appearing in the middle of the vision, more noticeable when vision is checked on the Amsler Grid.
What will your Ophthalmologist do if Wet AMD is suspected?
After a thorough clinical assessment, including a dilated examination of the macula, your ophthalmologist may arrange further testing for you. One test is an OCT (Ocular Coherence Tomography) scan of the macula. The scan is safe, painless, quick and provides the ophthalmologist with a high-resolution image of the macula. Repeat OCT scans are often used to monitor progress of treatment.
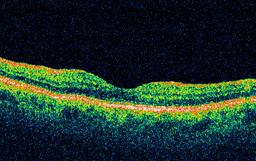
Normal OCT scan of the Macula
-
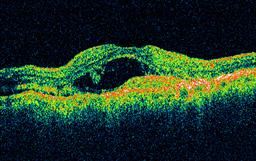
OCT scan of Wet AMD showing leakage and swelling
The other test your Ophthalmologist may require managing your AMD is a Fluorescein Angiogram.
What is a Fluorescein Angiogram?
Fluorescein angiography is a photographic test of the retina. A yellow dye called fluorescein is injected into a vein in your arm, where it travels through the body reaching the eye. A special camera uses bright flashes of light to take multiple photographs of the back of your eye as the dye passes through the blood vessels of the retina. In Wet AMD the dye will leak out of the abnormal blood vessel and it will show up as a bright spot on the photos. This angiogram not only makes the diagnosis, but it will tell us the size of the blood vessel and its location. This information will be used to determine the best treatment option.

Patient having a Fluorescein Angiogram
What are the side effects of Fluorescein Angiography?
After fluorescein angiography, your skin will turn yellow for several hours. This will fade as the dye is filtered out by the kidneys causing the urine to turn bright yellow for up to 24 hours. Your vision will be blurred, and you should not drive for the remainder of the day. There is no permanent effect on the vision from the test.
The chance of an adverse effect is low, but as with any medical procedure there are some risks involved. Some patients experience nausea during the angiogram. Some patients may vomit. Occasionally some fluorescein will leak from a fragile vein, which may cause a burning sensation and yellow staining of skin. The burning usually lasts a few minutes and the staining takes a few days to disappear.
Some patients may experience an allergic reaction to the fluorescein dye. The most frequent allergic reaction is a skin rash, which is often itchy and may appear within minutes after the fluorescein injection.
The most severe allergic reaction is called anaphylaxis, which is rare but may be life threatening. Very rarely patients may experience breathing difficulty or heart rhythm disturbances, which can be severe and even cause death. If you feel any itching, tingling in the lips or tongue, difficulty breathing or pain during or after the angiogram, let us know immediately. You may require medication to control the reaction, and your condition will be monitored until it has been resolved. Delayed reactions are rare.
How is Wet AMD treated?
If the blood vessel is small and located away from the centre of the macula, then it is possible to apply laser to seal off the blood vessel. However, there is a 50 percent chance that the blood vessel could grow back again.
Lucentis or Eylea Intravitreal Injections
Lucentis ( Ranibizumab) and Eylea (Aflibercept) are PBS-listed medications that are the treatment of choice for Wet AMD. The medication is injected into the eye and has the effect of stopping the growth of the abnormal blood vessel as well as reducing the amount of fluid leakage from it. Results from large, international studies of these medications show that most patients maintain or have improved vision. Only a small percentage do not respond to treatment and may lose vision.
Avastin Injections
Avastin (Bevacizumab) is registered as treatment for bowel cancer. However, due to its molecular similarity to Lucentis, it has been found to be just as effective in the treatment of Wet AMD. In this off-label use of Avastin, a small amount of the drug is injected into the eye. In certain cases of Wet AMD where Lucentis or Eylea is not PBS approved, Avastin can be considered.
How are Eye (Intravitreal) Injections given?
Firstly, anaesthetic eye drops are used. Then further anaesthetic can be delivered by an injection under the conjunctiva (the surface layer of the white of the eye). The eye is then washed with Betadine antiseptic to minimise the risk of infection. A fine 30-gauge needle is then inserted gently through the white part of the eye to deliver 0.05ml of either Lucentis or Avastin. The medication will then spread to the macula to "shut down" the abnormal blood vessel. In most cases an eye pad will be placed over the injected eye and a short course of eye antibiotics given.
What are the risks of eye injections?
The eye could be gritty and occasionally painful for the first 24 to 48 hours due to the drying effects of Betadine. This usually settles down with ocular lubricants, ointments and simple pain-killers (e.g. Paracetamol). Often, tiny air bubbles are injected into the eye which appear as round floaters or dark spots in the vision. Again, this is harmless and should disappear over the next few days.
Serious sight-threatening complications are fortunately rare, and they include infection (endophthalmitis), bleeding and retinal detachment. The risk of infection, for example is 1 in 2000. Injury to the lens can result in cataract. Emergency eye surgery may be needed to the save the sight in this situation.
How frequent and how long is the course of injections?
Lucentis and Avastin in the eye wears off 4 weeks after the injection. Therefore, in the initial phase, the injections need to be given every 4 weeks. When the blood vessel appears to be under control, treatments can be extended. Although there are obvious benefits in spreading out the injections, there is also the risk that the blood vessel may reactivate, leading to further leakage and bleeding which can in turn affect the vision permanently. Treatment has to be individualised for each patient.
Currently, the evidence supports ongoing treatments indefinitely. The patient can decide to stop treatment for various reasons but there is a risk that the vision could worsen if the blood vessel reactivates sometime in the future. It is important to discuss any decision to stop treatment with your Ophthalmologist first.
What is the risk of Wet AMD in the good eye?
There is a 50 percent chance that the "good" eye will develop Wet AMD. Therefore, it is essential that the patient monitors the vision in the good eye with the Amsler grid and report any new or increasing distortion promptly to the Ophthalmologist. Vitamin and Zinc supplementation works best in this situation to reduce the risk of Wet AMD in the good eye. Speak to your ophthalmologist about this.
Focal Laser
If the blood vessel is small and located away from the centre of the macula, then it is possible to apply laser to seal off the blood vessel. However, there is a 50 percent chance that the blood vessel could grow back again.
You will need the Adobe Reader to view and print these documents.
![]()