Keratoconus
Keratoconus is a degenerative disorder of the cornea, the clear focusing surface at the front of the eye. The cornea is normally a dome or soccer ball shape and this shape changes in keratoconus to a more irregular cone or rugby ball shape. This leads to poor vision that often cannot be fully correctable with glasses. People with this condition often complain of glare or haloes or double vision as well as blurry vision.
What causes keratoconus?
The exact cause of keratoconus is unknown. It is genetic but not everyone who has the gene will have keratoconus. So, there will be some families where mum or dad has it and all the kids have it or some families where only one person has it. Allergies and eye rubbing are also thought to play an important part. Therefore, it is recommended that allergies are treated and people with keratoconus avoid rubbing their eyes.
Who gets keratoconus?
Typically, keratoconus comes on in your teenage years and stabilizes in your mid 20’s to early 30’s. Most people have had it for months to years before being diagnosed because young people can compensate for their blurred vision by adjusting their focus with the internal zooming lens of their eye.
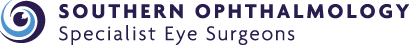
Bent light beam from microscope shows the abnormal shape of the cornea.
How is it diagnosed?
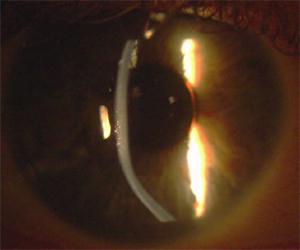
Your optometrist or ophthalmologist may suspect you have keratoconus if your vision is getting worse and your astigmatism increasing. There are also certain signs they can see when they examine you on the slit lamp microscope. However, the best test is corneal topography or mapping. This machine will show the abnormal shape of the cornea in precise detail.
Corneal topography or mapping shows the abnormal shape displayed as red colours.
How is keratoconus treated?
There are two main problems that need to be addressed with keratoconus:
- Ongoing deterioration
- Poor vision
Stopping deterioration
Corneal Collagen Crosslinking is the only treatment available to stop keratoconus from deteriorating further. It involves hardening or strengthening the cornea with vitamin B2 (riboflavin) and UV light. The success rate of Crosslinking is about 95% at stopping keratoconus getting worse. It does not generally improve the vision.
Treating poor vision
In the early stages of keratoconus, spectacles may be all that is required to correct the visual aspects of keratoconus.
As the disease progresses rigid (hard) contact lenses may be prescribed. These are made from a special material that allows the contact lens to 'vault' over the cornea, neutralising the effect of the irregular shape and improving vision.
Surgery treatments are only used if contact lenses cannot be worn or tolerated. Surgery options include:
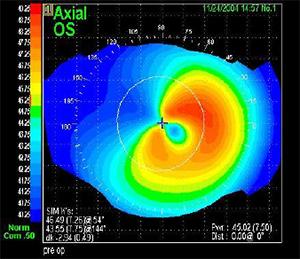
- The surgical insertion of ring segments. This involves inserting clear plastic segments into the cornea. These segments are designed to reshape the front surface of the eye, thus correcting refractive errors caused by keratoconus. The two main brands of rings are Intacs or Kera rings.
- Corneal transplantation. This will only be suggested once all other treatments have been exhausted. About 10-20% of patients eventually require corneal transplantation.
Rings are surgical plastic implants Inserted using a laser to reshape the abnormal cornea.